How Pelvic Physical Therapy Can Help Improve Sexual Function After Surgery
Pelvic surgery is sometimes required as part of treatment and management for gynecological and colorectal issues.
These may include surgery as part of cancer treatment, hysterectomy, uterine fibroids removal, endometriosis excision, laparoscopic procedures and pelvic organ prolapse procedures.
It is not uncommon to have issues related to sexual functioning after undergoing such procedures. Potential symptoms you may experience include dyspareunia (pain with intercourse), feelings of vaginal tightness, vaginal scarring and vaginal shortening as well as difficulties related to desire, arousal and orgasm (Carberry, Antosh & Rogers, 2019).
Although these complications may seem intimidating, there are many ways that a pelvic floor therapist can help to improve sexual functioning after pelvic surgery.
Tight? Start here!
Pelvic Physical Therapy Treatment
Pelvic physical therapy is a specialized form of rehabilitation for abdominal and pelvic floor dysfunction. Physical therapists who pursue this area must complete additional training beyond their physical therapy degree.
During your first visit, the therapist will explain that the pelvic floor consists of muscles, ligaments and other tissues that work in harmony with muscles in the abdomen to control your breathing, bowel, bladder and sexual functioning.
A pelvic floor therapist will evaluate how your abdomen and pelvic floor work together by using gentle internal and external examination and treatment techniques.
The goal of treatment is to address any disruptions in the system that may be causing tightness or weakness of muscles. The pelvic physical therapist will ask questions about pain, bowel or bladder issues or problems related to sexual functioning.
If pelvic surgery is needed, a pelvic physical therapist can work with you to help you heal after surgery.
Rehabilitation
Generally, pelvic rehabilitation will begin 6-8 weeks following the surgical procedure. If radiation is utilized following surgery for cancer treatment, this timeline is often extended until after radiation is complete.
The pelvic physical therapist will go over your medical history and will ask in-depth questions about your bladder, bowel and symptoms associated with sex.
Because each of these systems are housed in the pelvic bowl and many times share common nerves, it is important for the pelvic therapist to get a good sense of how each system is functioning for you.
They may ask you to keep a bladder or bowel diary for 2-3 days and will ask what your goals are. The therapist will also conduct a thorough examination of your back, hips, abdomen, pelvis and pelvic floor.
Generally, a brief intra-vaginal examination will take place to determine your pelvic floor muscle strength, endurance, coordination and flexibility.
They will also look at how well the vaginal tissue and pelvic floor have healed following surgery and will base your plan of care on their findings.
Tools That Help With Pelvic Pain After Surgery
In addition to pelvic floor rehabilitation there are tools that can be used to help decrease pain and improve your ability to participate in and enjoy sex again.
These tools can often be used independently or in conjunction with other treatments. They include vaginal dilators, also referred to as vaginal trainers, pelvic wands and healing balms.
Vaginal Dilators
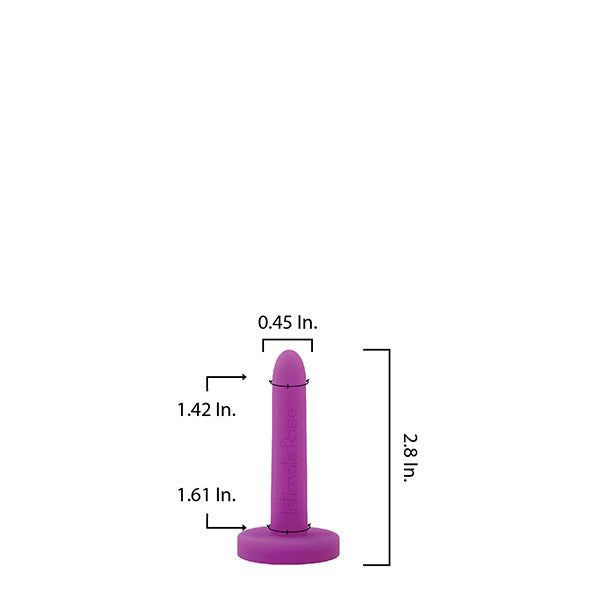
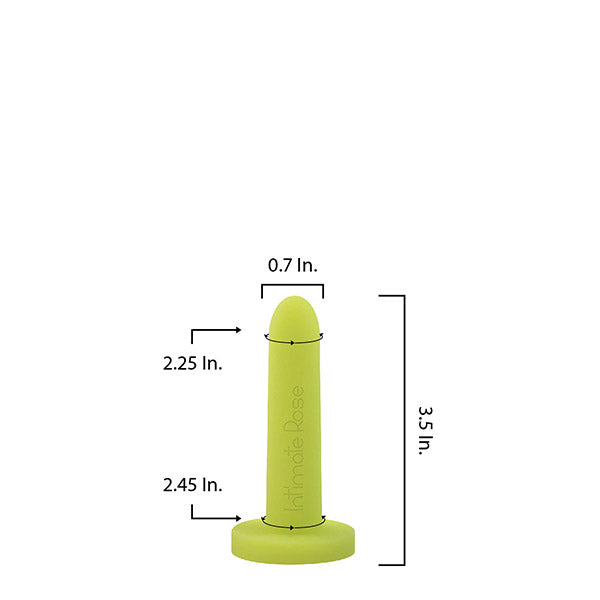
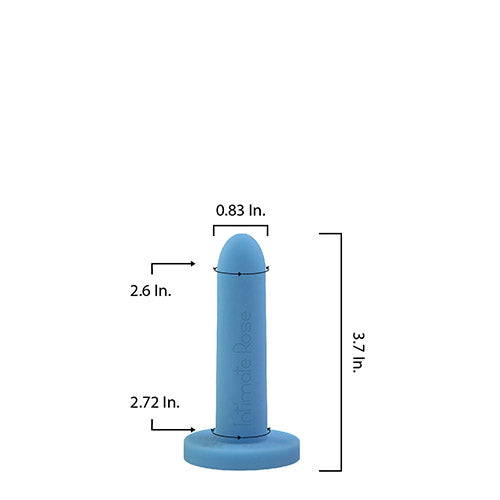
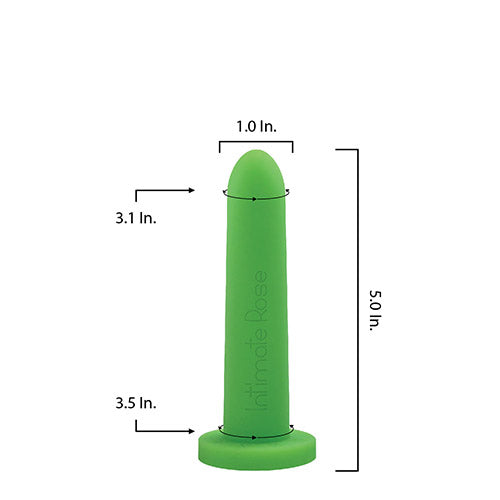
Vaginal dilators come in various sizes and materials with the best being made from medical-grade silicone and coming in progressively larger sizes.
As with any surgery, scar tissue and adhesions can form within and around the surgical area as the body heals, which can contribute to pain with penetration.
The use of vaginal dilators will help to gently stretch the vaginal canal increasingly over time with the ultimate goal of improving pelvic floor muscle and tissue elasticity, coordination and relaxation.
Your pelvic PT will help you find the right size dilator to start with, teach you proper use and help you form a routine plan for when you will use them. After your body can move comfortably in a variety of positions while using the initial dilator, you can progress to the dilator size.
Implementing vaginal dilators into your postoperative treatment plan will help you move one step closer to restoring your sexual functioning or ability to tolerate a medical examination without pain.
How does a vaginal dilator work?

Pelvic Floor Wands
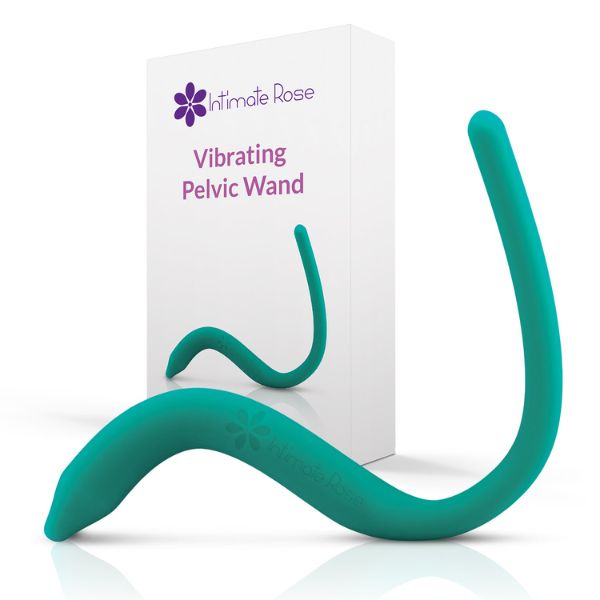
One of the common side effects following pelvic surgical procedures is tightness in the pelvic floor muscles, which can lead to areas of tension and discomfort.
If left untreated, this muscle tightness can contribute to other issues such as chronic pelvic pain. A pelvic floor wand is another tool used in pelvic physical therapy that can help address these painful areas
The exclusively patented Intimate Rose pelvic wand, covered in smooth medical-grade silicone, may be inserted vaginally or rectally. Designed for targeted relief, its unique shape allows easy access to both superficial and deep pelvic floor muscles, helping to ease minor aches and discomfort.
The vibrating version offers ten different vibration settings to promote circulation, relaxation, and support for sexual wellness.
This tool can be a great addition to pelvic physical therapy and can help to provide relief from aches and pains in the comfort of your home following surgery.
Balms
Vaginal Balms can be used to help promote healing in the vulvar tissue after surgery. Following pelvic or abdominal surgery or radiation the skin in the vulvar region and area surrounding the vagina can become irritated or dry.
A moisturizing balm such as Intimate Rose’s Enchanted Rose feminine balm can be applied to the area just as you would use chapstick to help heal dry or irritated skin on the lips and mouth.
The balm can be applied as often as you need and is made of organic ingredients by a pharmacy team.
References
Carberry, C., Antosh, D., & Rogers, R. (2019). Assessing and treating sexual function after vaginal surgery: Keys to treatment include knowing the patient’s preoperative: history of any dysfunction; understanding her concerns, needs, and expectations; and starting conservatively. OBG Management, 31(5), SS2–. https://cdn.mdedge.com/files/s3fs-public/issues/articles/obgm03105ss1_ss15.pdf

Tight? Start here!