Pelvic floor dysfunction is an overarching condition that includes many disorders that are affected by the pelvic floor.
Your pelvic floor muscles sit between your two hip bones and act as a sling to support your bladder, rectum, and sexual/reproductive organs to assist with urination, defecation, sexual, reproductive functions and contribute to a healthier vagina.
Types of Pelvic Floor Dysfunction
- Difficulties with bladder or bowel control
- Pain or lack of sensation with intercourse
- Pelvic pain/chronic pelvic pain
- Prolapse
With each of these disorders, the underlying problems can be caused by overactivity or under-activity of the pelvic floor.
Overactivity of the pelvic floor, also known as hypertonic disorders, are caused by too much activity of the muscles or decreased ability to relax. Under-activity of the pelvic floor, or hypotonic disorders, are caused by weak or shortened muscles. (Stein, Wallace)
Common Symptoms & Conditions Associated with Overactive Pelvic Floor Disorders
- Bladder: urinary urgency, frequency, and/or retention, interstitial cystitis
- Bowel: constipation, irritable bowel syndrome (IBS)
- Sexual dysfunction: difficulty reaching orgasm, hyperarousal disorder, dyspareunia, post-ejaculartory pain, postpartum sexual dysfunction
- Pelvic Pain/Chronic Pain: coccygodynia, hip/groin/SI pain, pelvic girdle pain, pelvic floor tension myalgia, vaginismus, vulvodynia, penile/testicular or vaginal pain, endometriosis, prostatitis
Common Symptoms & Conditions Associated with Underactive Pelvic Floor Disorders
- Bladder: urinary incontinence (stress and/or urge incontinence), overactive bladder
- Bowel: fecal incontinence, involuntary loss of gas
- Sexual dysfunction: decreased arousal, decreased sexual response, erectile dysfunction
- Prolapse: cystocele (bladder), enterocele (small intestine), rectocele (rectum), uterine
Prevalence of Pelvic Floor Dysfunction
The prevalence of at least one pelvic floor disorder in women over the age of 20 is approximately 24% in the United States of America.
Roughly one third of women with symptomatic pelvic floor disorders had more than one disorder.
Treatment for Pelvic Floor Dysfunction
Medical guidelines recommend using conservative treatments including behavior modification and pelvic floor physical therapy as the starting point for treatment for pelvic floor dysfunction. (Arnouk)
Guides
Pelvic floor physical therapy has been proven to be effective in treating both overactive and underactive pelvic floor disorders and helping with lower back pain from pelvic floor disorders.
 Overactive pelvic floor disorders that can benefit from physical therapy include pelvic pain, pain with intercourse (dyspareunia), vaginismus, vulvodynia, and postpartum sexual dysfunction.
Overactive pelvic floor disorders that can benefit from physical therapy include pelvic pain, pain with intercourse (dyspareunia), vaginismus, vulvodynia, and postpartum sexual dysfunction.
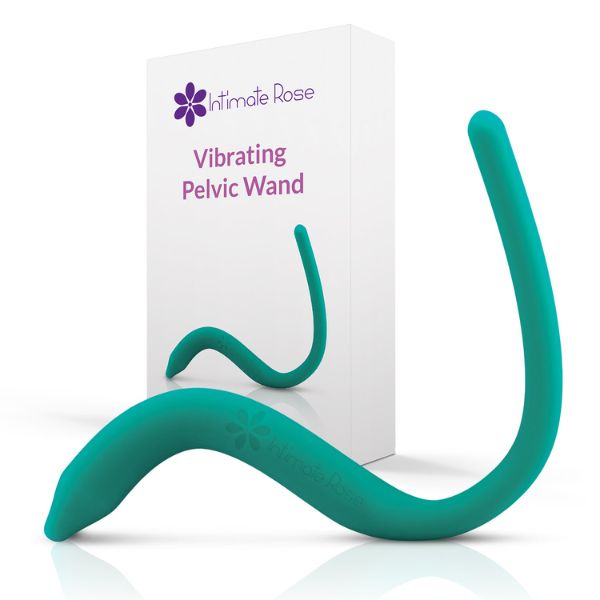
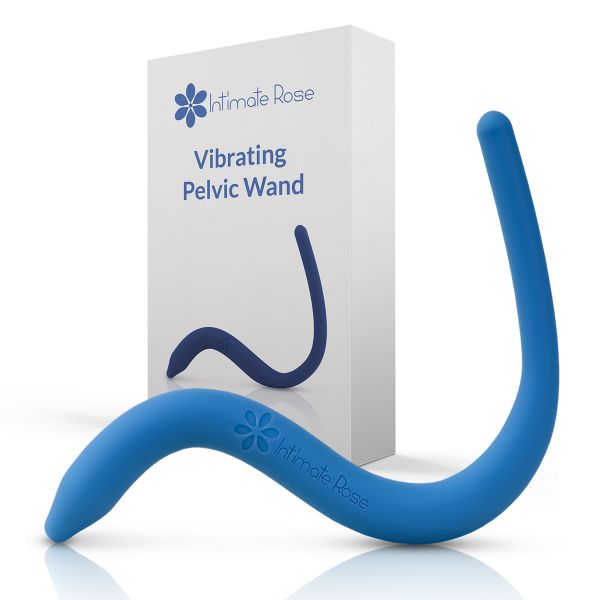
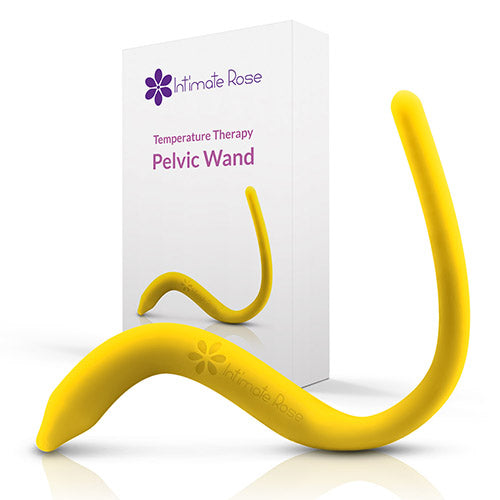
Pelvic wands are commonly recommended for people with overactive pelvic floor muscles dysfunction to provide release to the muscles and eliminate trigger points and tender points.
Dilators are commonly recommended for people who have pain with tampons, medical exams or intercourse.
Underactive pelvic floor disorders that can benefit from physical therapy include stress urinary incontinence, pelvic organ prolapse, anal and fecal incontinenece, postpartum pelvic organ prolapse and urinary incontinence. (Wallace) Vaginal weights (Kegel weights) are commonly recommended for people with underactive pelvic floor muscle dysfunction to help train and improve strength of the muscle.
When choosing a physical therapist, ensure that they have received specialized training in pelvic floor dysfunction for optimal treatment results.
 Physical therapy treatments may include pelvic floor exercises, postural changes, strengthening or stretching, biofeedback, manual therapy, education, and instructions on medical devices such as vaginal weights or dilators as appropriate.
Physical therapy treatments may include pelvic floor exercises, postural changes, strengthening or stretching, biofeedback, manual therapy, education, and instructions on medical devices such as vaginal weights or dilators as appropriate.
Consult with your provider to explore whether Intimate Rose’s collection of patented Pelvic wands, dilators, or Kegel weights might be right for you.
You may benefit from treatments other than conservative management depending on your response to physical therapy and behavior modification including medications or surgeries which can be recommended by an appropriate health care provider including your primary care physician, OB/GYN, or urologist.
Do Men Also Suffer from Pelvic Floor Disfunction?
Men also can suffer from pelvic floor dysfunction however the overall prevalence in the United States has not been well established.
There are several well-known risk factors for pelvic floor dysfunction including age, gender, childbirth including number of births and type of birth, and obesity/body mass index.
Pelvic floor dysfunction should be considered a chronic disease due to potential presence throughout the lifespan and change with age. (Hallock)
More men's health content? Be sure to check out our dedicated men's health section.
Are Pelvic Floor Disorders Common?
The prevalence of pelvic floor dysfunction increases greatly with age. For example, 9.7% females between the ages of 20 and 39 experience one or more pelvic floor dysfunctions and this proportion increases steadily by age until 49.7% of females over the age of 80 experience one or more of these disorders.
Due to females having a longer lifespan than men on average, more women are likely to suffer from pelvic floor dysfunction. (Luber)
Additionally, women have a higher prevalence of pelvic floor dysfunction than men due to giving birth.
However even excluding childbirth, females who have not given birth are 3x more likely to experience stress urinary incontinence than men indicating that gender greatly affects likelihood of pelvic floor disorders. (Luber)
Is Pelvic Floor Dysfunction More Common in Women?
The prevalence of pelvic floor dysfunction in women increases with the number of deliveries and type of delivery as more vaginal births tends to result in increased likelihood of pelvic floor disorders.
One study by Nygaard et al found that the percentage of women who experience pelvic floor dysfunction was 12.8% for women with 0 children, 18.4% for women with 1 child, 24.6% for women with 2 children and 32.4% for women with 3 or more children. (Nygaard)
Lastly higher body mass index and obesity are risk factors for prolapse and both urinary and fecal incontinence.
Obesity has been shown to increase incontinence symptoms as an individual ages. The proportion of women with at least one pelvic floor disorder was found to be 75% for obese women versus 44% in non-obese women. (Hallock)
Race, genetics and socioeconomic status have not been shown to be risk factors for pelvic floor impairments at this time but further research is being conducted.
References
Stein A, Sauder SK, Reale J. The role of physical therapy in sexual health in men and women: Evaluation and treatment. Sex Med Rev 2019;7:46–56.
Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: Current observations and future projections. Presented at the Sixty-seventh Annual Meeting of the Pacific Coast Obstetrical and Gynecological Society, Kamuela, Hawaii, November 14-19, 2000.
Hallock, J. L., & Handa, V. L. (2016). The Epidemiology of Pelvic Floor Disorders and Childbirth: An Update. Obstetrics and gynecology clinics of North America, 43(1), 1–13. https://doi.org/10.1016/j.ogc.2015.10.008
Ingrid Nygaard MD et al. Prevalence of Symptomatic Pelvic Floor Disorders in US Women. Journal of the American Medical Association, September 17, 2008—Vol 300, No. 11
Arnouk, A., De, E., Rehfuss, A. et al. Physical, Complementary, and Alternative Medicine in the Treatment of Pelvic Floor Disorders. Curr Urol Rep 18, 47 (2017). https://doi.org/10.1007/s11934-017-0694-7
Wallace, S. L., Miller, L. D., & Mishra, K. (2019). Pelvic Floor Physical Therapy in the Treatment of Pelvic Floor Dysfunction in Women. Wolters Kluwer Health, Inc, (2019).
Pelvic Wands